By Dr. Chris Tonozzi, MD, Director of Data Quality
Health care providers at Mountain Family Health Centers see lots of hardworking patients come through our doors, so when I first heard that health care field is facing a crisis related to provider burnout, I felt chagrined when I compared our privilege to that of our hardworking patients. After all, providers are respected, high-paid professionals. But the data that is being assembled nationally reveals that there are some serious concerns at hand.
When I say “provider,” I am referring to doctors, nurse practitioners and physician assistants. Burnout for medical professionals is conceptualized as follows (source):
- Emotional Exhaustion: tiredness, feeling poorly physically, low emotional resources, and feeling that one has nothing left to give to others.
- Depersonalization: negative, cynical attitudes and impersonal feelings toward clients.
- Reduced Personal Accomplishment: a feeling of incompetence, inefficiency or inadequacy.
Here is a conceptualization of the drivers, or sources, of provider burnout (source).
A 2015 article in the Mayo Clinic Proceedings showed that between 2011 and 2014 the percentage of providers experiencing at least one symptom of burnout rose from 45.5% to 54.4%. Provider satisfaction with work-life balance decreased from 48.5% to 40.9% over the same period. And compared to the general population, even adjusted for things like age, gender, relationship status, hours worked per week, providers are found to experience professional burnout twice as often as professionals.
The impacts of this are significant. Providers are leaving the profession (to retirement or career changes) exacerbating the shortage of primary care providers. The patient experience is obviously impacted when burnout is significant; patient visits are less pleasant. There are fears (and some data) that the quality and safety of the care provided is affected. Additionally, there is a significant cost to provider burnout. The American Medical Association (AMA) estimates that for a 30-provider practice, the annual cost of provider burnout is $368,000, mostly related to turnover costs.
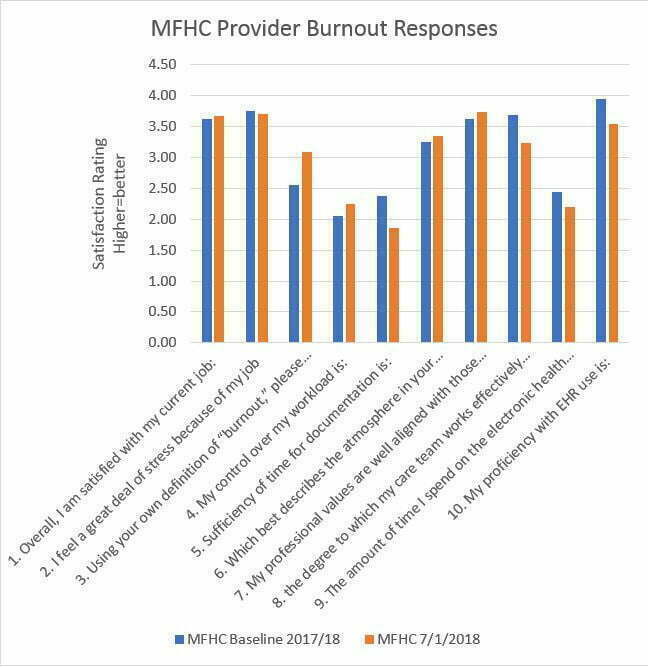
A common provider burnout survey is called the “Mini Z.” Presented below are the responses that Mountain Family providers gave for the Mini Z survey during late 2017/early 2018 and then when surveyed again in July 2018. We see that there is concern in the areas of “control of my workload,” “sufficiency for time for documentation,” and “the amount of time I spend on the electronic health record.”
What are we doing and what more can we do about provider burn-out? The Stanford Wellness Framework has developed three strategic areas.
- Culture of Wellness. Mountain Family has made strides in measuring wellness of providers, like the Mini-Z Assessment above. Mountain Family’s Human Resources also tracks an “Index of Wellbeing” that is often used for strategic planning by Mountain Family leadership. We promote “self-care” by offering Wellness Hours in which volunteer or health promoting activities are incentivized by giving paid time off in exchange for these activities. Other areas that Stanford Wellness Framework emphasizes are engaging senior leadership and strengthening local leadership.
- Efficiency of Practice. Mountain Family practices are adopting “Team Based Care” which organizes providers, nurses, medical assistants and others into cohesive teams where work is more efficiently delegated between members. Also important in this arena is improving Electronic Health Record Function. As is clear from the Mini-Z Assessment, we’ve got work to do.
- Personal Resilience. The majority of provider well-being is driven by systems factors within health care, but it is also important to support self-care of providers. We promote “self-care” by offering Wellness Hours in which volunteer or health promoting activities are incentivized by giving paid time off in exchange for these activities. We need to be on the lookout for more opportunities in this regard.
Mountain Family Health Centers has made strides in supporting the well-being of all employees, but it’s clear that providers are facing particular obstacles. We have provider leaders working hard to find solutions. Our long-term stability will depend on these efforts.